- Posted
- Categories
-
- OpenPrescribing
OpenPrescribing Hospitals email alerts
Stay updated with notifications of new OpenPrescribing Hospitals features and data releases.
Stay updated with notifications of new OpenPrescribing Hospitals features and data releases.

We’re excited to open registration and submissions of ideas for the 2025 Bennett Institute Medicines Symposium, a two-day event that brings together everyone working with NHS medicines data.

This newsletter contains all the latest updates from OpenPrescribing

A look at how to run a multi-product analysis on OpenPrescribing Hospitals.

How to choose the most appropriate quantity type for custom analyses on OpenPrescribing Hospitals.

A look at how to use the summary tables produced in custom analyses on OpenPrescribing Hospitals.

In this guest blog James Galloway a Professor of Rheumatology and an Honorary Consultant Rheumatologist in South London, at King’s College London describes how his team used OpenPrescribing to reduce unsafe methotrexate prescribing and shares his thoughts on improving quality of care may deliver most improvements for the populations health.

How you can run custom analyses of variation in medicines issuing across NHS trusts, ICB, region and nationally.

A summary of our research letter highlighting continuing co-proxamol use, published in the British Journal of General Practice

A national medicines usage analysis for lithium in primary and secondary care in England

We’ve launched a new OpenPrescribing Hospitals ‘low value prescribing’ measure for lidocaine plasters.

Special edition OpenPrescribing newsletter introducing our new tool, OpenPrescribing Hospitals.

We’re launching the Bennett Prize in OpenPrescribing to celebrate the best user-led projects using OpenPrescribing. Enter by sharing your work online and sending us the link — all kinds of entries welcome, from prescribing insights to data science deep dives.

What are biosimilars, why are they of interest and why can we monitor usage with primary care data but not secondary care data?

In this guest blog, Dr Christianne Micallef explains how she uses OpenPrescribing in her role as an antimicrobial stewardship lead pharmacist.

A look at the new Product Lookup feature on OpenPrescribing Hospitals

What is a Defined Daily Dose, how can they calculated from the quantity reported in the Secondary Care Medicines Data, and why are they useful?
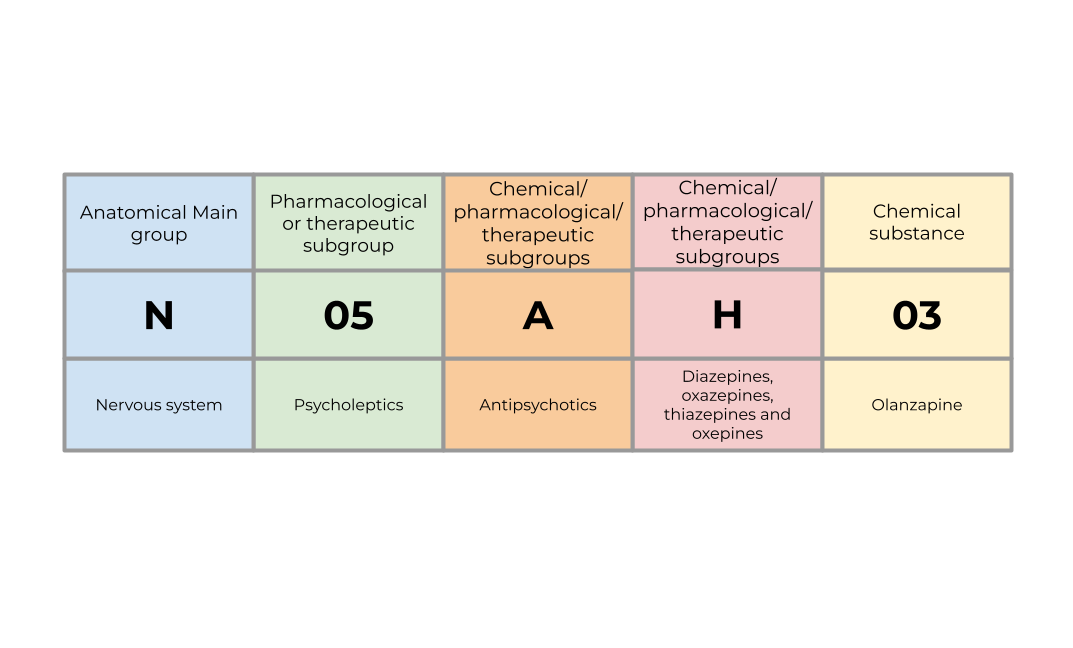
How the ATC can be used to classify medications and how DDs can be used to measure their usage.

What is ingredient quantity, how can it be calculated from the quantity reported in the Secondary Care Medicines Data, and why is it useful?
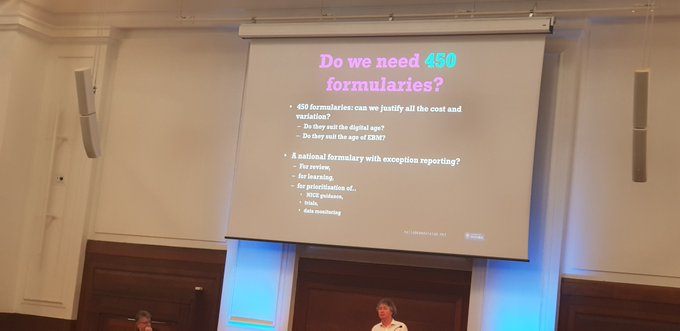
In 2019, we pitched a national tool to track local formularies. Now the NHS is doing just that! We’re sharing our plans and advice to help it succeed.

What are unit doses, how can they be calculated from the quantity reported in the Secondary Care Medicines Data, and why are they useful?
A look at how quantity is measured in the Secondary Care Medicines Data

The new custom analysis feature on OpenPrescribing Hospitals.

How we can use OpenPrescribing Hospitals measures to look at use of low value medicines in hospitals.
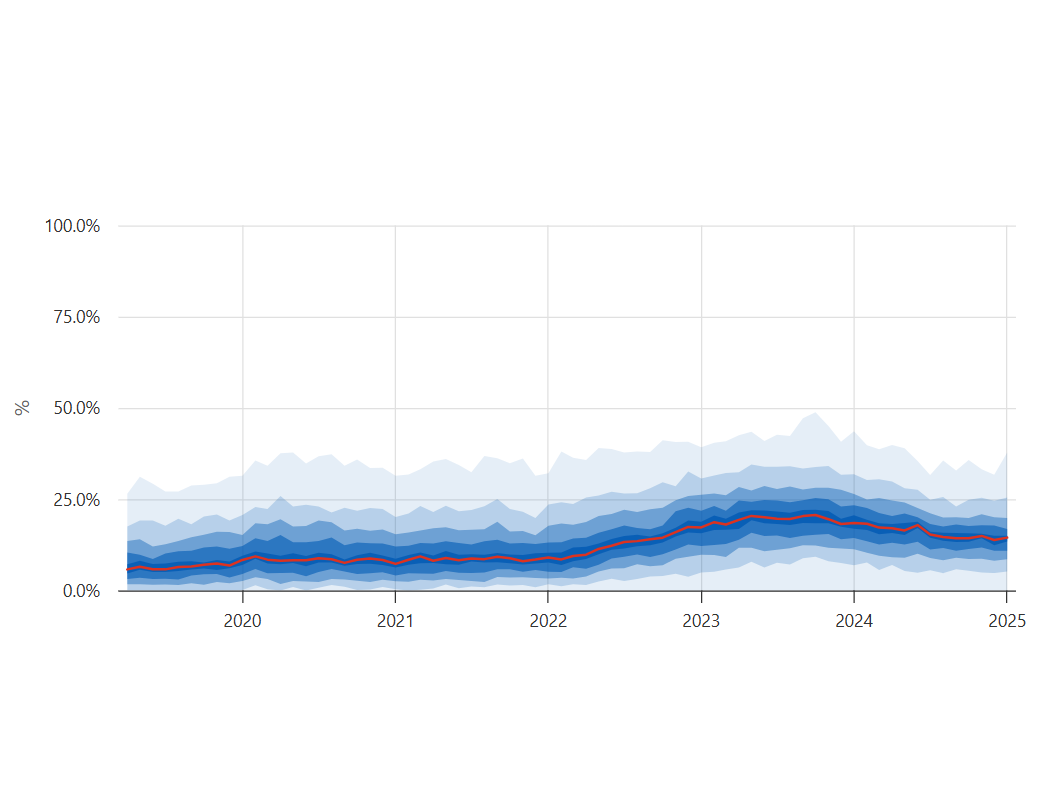
How we highlight variation in hospital medicines usage in OpenPrescribing Hospitals Measures.
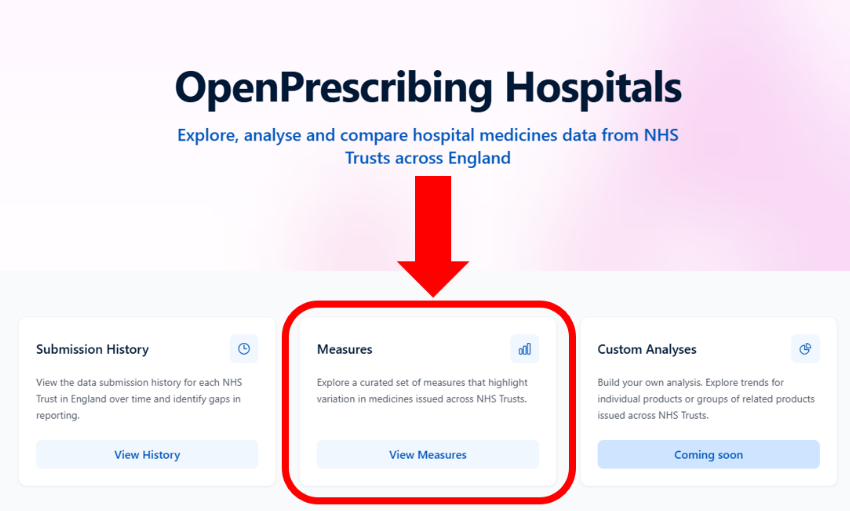
An introduction to a new measures tool in OpenPrescribing Hospital.
The way the Secondary Care Medicines Data is published has recently changed. This is why this is good news for OpenPrescribing Hospitals.

This blog explains the major changes we’ve made to how the Price-Per-Unit tool works
How we can make it easier to compare issuing quantities of different products within the Secondary Care Medicines Data by using the dictionary of medicines and devices to find more detailed product information.

A first look at the data within the Secondary Care Medicines Dataset.

We’ve made OpenPrescribing Hospitals platform to all with our first feature. Read more to see how you can access it.

A deeper dive into what stock control data is and how it impacts the way the SCMD is published
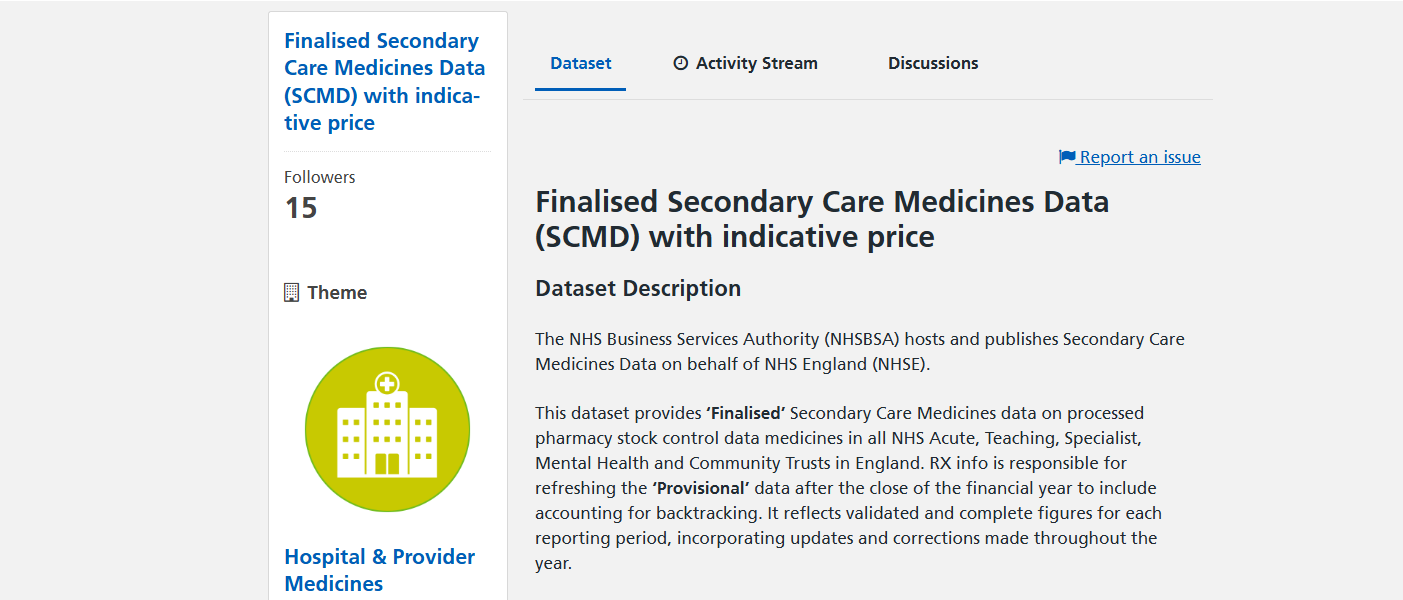
A brief description of the Secondary Care Medicines Dataset, the primary dataset used in OpenPrescribing Hospitals
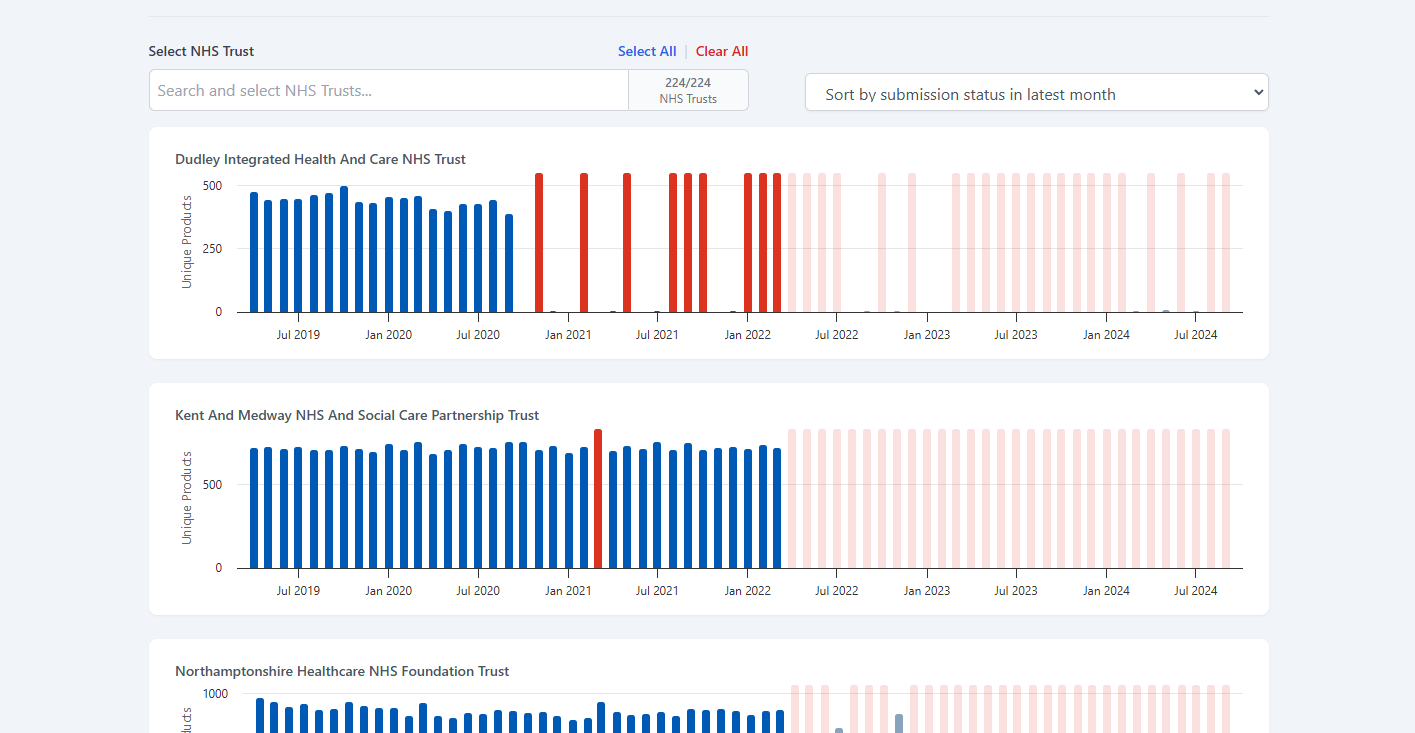
An explanation of the Submission History feature on OpenPrescribing Hospitals
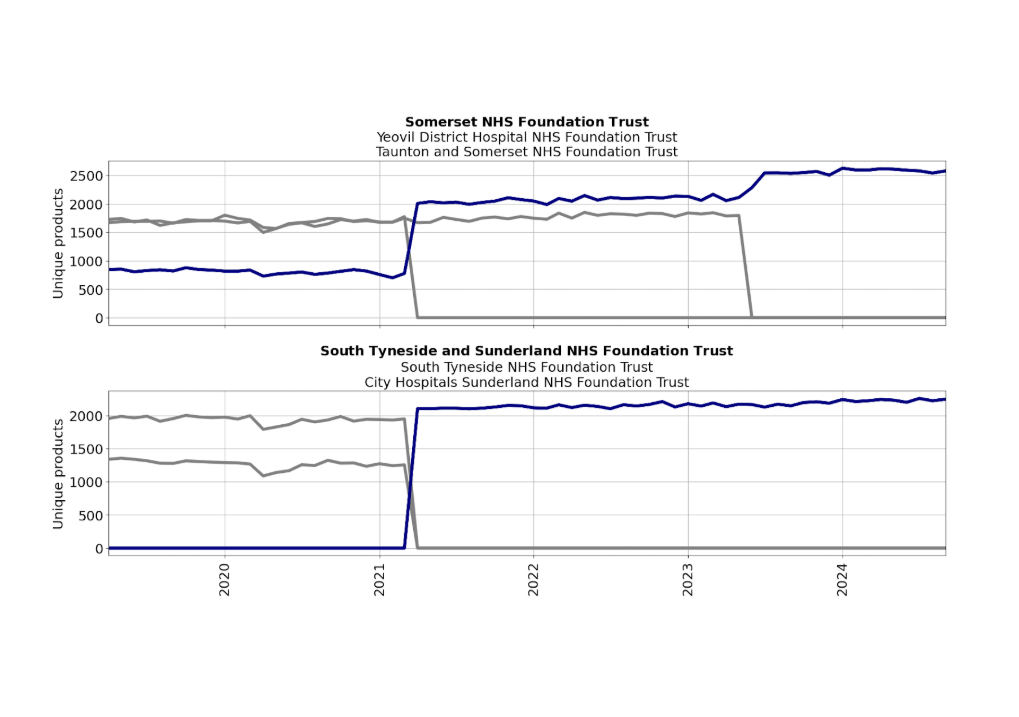
The third blog in the series: Organising Organisations. Here, we describe how consistent the data submitted by NHS Trusts to the Secondary Care Medicines Dataset is
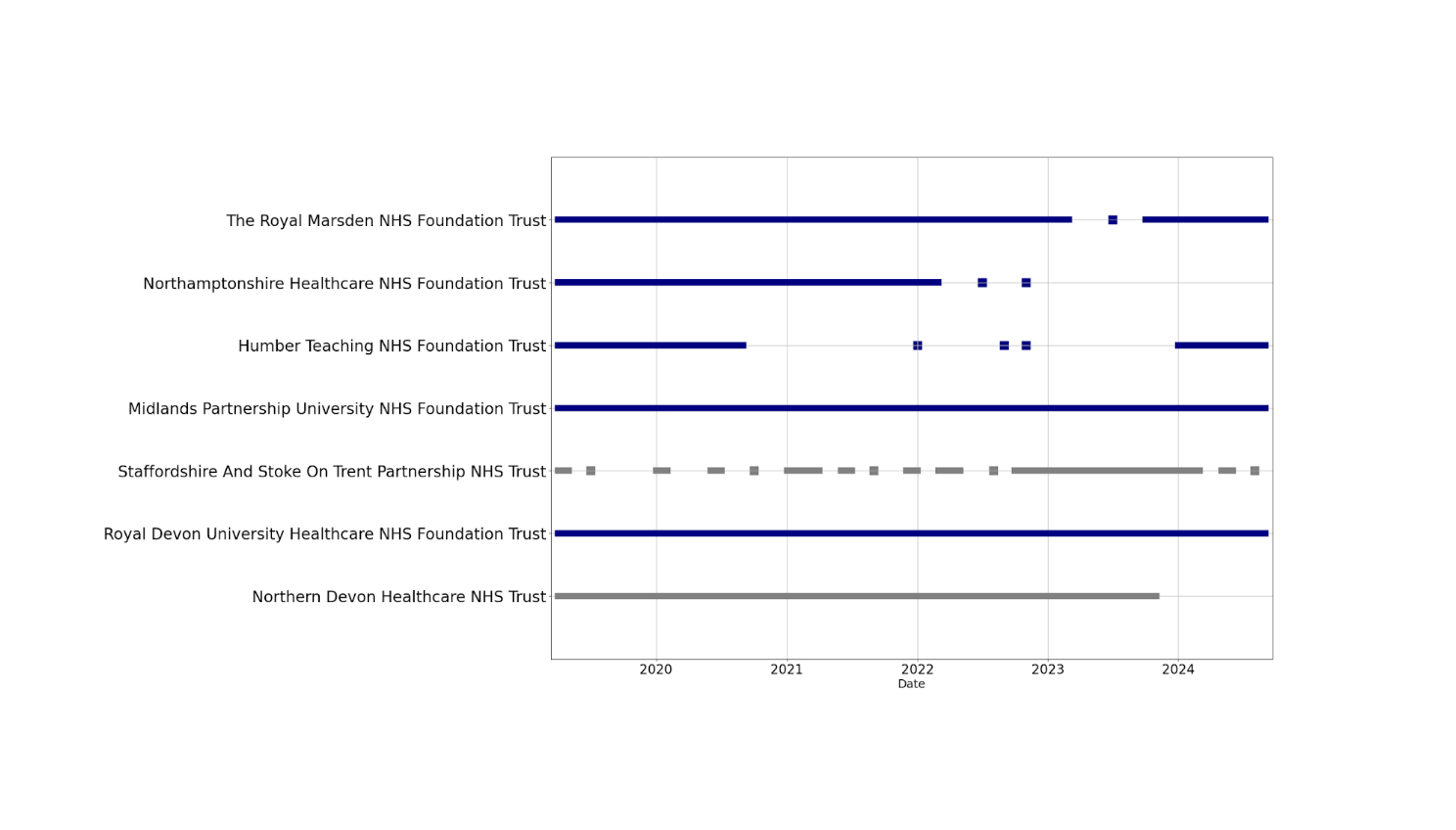
The second blog in the series: Organising Organisations. Here, we describe how complete the data submitted by NHS Trusts to the Secondary Care Medicines Dataset is

The first blog in the series: Organising Organisations. Here, we describe which NHS Trusts are included in the Secondary Care Medicines Dataset and how they can be identified

Here we describe how to access and use the Low Value Prescribing dashboard on OpenPrescribing.

We’re going to build OpenPrescribing for hospitals using openly available secondary care medicines data. Here we explain why and what you can expect.

If you didn’t manage to attend the OpenPrescribing antimicrobial stewardship webinar, don’t worry! You can watch it back here.

This newsletter contains all the latest updates from OpenPrescribing.
Catch up with our OpenPrescribing webinars

We are hosting a webinar special in support of World Antimicrobial Resistance Awareness Week 2024

We’ve analysed what we know about our OpenPrescribing user base. Here’s some information obout how many of you there are, what you all look at, and which organisations have signed up to our alerts.

We’ve updated the DOAC measure following changes to the NHS England commissioning guidance.

We briefly summarise all the recent big and exciting developments in hospital medicines data.

This newsletter contains all the latest updates from OpenPrescribing

We’ve been producing estimates on the impact of Price Concessions since 2017. In this blog we describe the changes we’re making in how we estimate the costs.

We’re setting up webinars for different groups to show how to use OpenPrescribing effectively. Each session will cover the basics and tips for getting the most out of it.

We describe the reasons why people sometimes find a medicine on OpenPrescribing.

In this guest blog, Molly Mattsson describes how we compared lidocaine prescribing reduction policy implementation in Ireland and England.

This newsletter contains all the latest updates from OpenPrescribing

We’ve launched a new OpenPrescribing tool, the Improvement Radar, which makes it easy to identify organisations which have shown substantial improvement.

In this blog we explain some of the issues with using STAR-PUs and ask for your input on how we should use them in future.

This newsletter contains all the latest updates from OpenPrescribing

In the second of a two-part blog we explain why OpenPrescribing figures don’t always match with other prescribing data resources, due to differences in how data is presented.

In the first of a two-part blog we explain why OpenPrescribing figures don’t always match with other prescribing data resources, due to differences in the data source.

This blog describes how we develop new measures at OpenPrescribing.

The second session in the Bennett Conference was a series of talks covering the history, technical underpinnings, research and use cases of OpenPrescribing.

A whistlestop tour of the whole history of our group, from OpenPrescribing via TrialsTracker to OpenSAFELY and on through Open Science, policy work, and more

A common question asked of the Bennett Institute is ‘have you got a tool to map BNF codes to dm+d codes?’ We’ve created one to download

We’ve been busy creating new measures for OpenPrescribing.net, and reviewing ones which aren’t needed any more.

We’ve been busy doing housekeeping on OpenPrescribing.net measures. Here’s a summary of the main changes.

OpenPrescribing Autumn 2023 Newsletter.

In this blog, we describe how OpenPrescribing tools helped identify and investigate a sudden £450k per month increase in NHS expenditure

In this blog we describe how to use and access the NHS England Medicines Optimisation Oppurtunitites dashboard on OpenPrescribing

At the Bennett Institute for Applied Data Science we’re always pleased to see stories in the media which have used OpenPrescribing.net. Here are some of the highlights of stories that we have been featured in recently.

Here we introduce the Bennett Institute’s Clinical Informatics team, explaining what they do and how their experience in NHS clinical practice helps them do this.

One of our key aims at Bennett Institute for Applied Data Science is to develop novel data-driven approaches to interpret our health care data. We want to use data science to identify patterns in the data that afford us a new, unbiased perspective on how well the NHS is working and how it could be better.

Bennett Institute resident pharmacist Brian MacKenna sets out some brief information on how we currently build medicines codelists on OpenSAFELY.

Our latest newsletter including information on: Bennett Institute for Applied Data Science, we are recruiting, Goldacre Review, updated Outlier Dashboards, recent changes to OpenPrescribing Measures, OpenSAFELY news, and new data news.

We have a new tool available at OpenPrescribing: our outlier prescribing dashboards will show you what your favourite CCG, PCN, STP or practice are prescribing more (or less) than everyone else. Read more about how it works and how to use it here.

Our latest newsletter including information on: We are recruiting, recent changes to OpenPrescribing Measures, new Outlier Prescribing tool, maps update, recent research publications, OpenSAFELY news, and new data news.

Recently we started reviewing a number of measures that needed the most urgent attention. As a result a number have been updated and a couple have been retired.

Our latest newsletter including information on: new job roles, hospital only measure, total oral morphine equivalence measures, OpenPrescribing and Bennett Institute Papers.

We have been very busy since our last newsletter back in July and there are tonnes of exciting updates for you here!
The Faculty of Pain Medicine has recently updated their recommendation on oral morphine equivalence (OME) which we use on our OpenPrescribing measure of OME. We have taken this opportunity to update and a new novel implementation of how we assess OME. Until this work is completed we have taken the decision to “suspend” the measure from dashboards however you can still view the old method using this link.

In July, Ben and Brian wrote a piece in the British Medical Journal arguing that hospital medicines data should be openly shared. Magnificently, the NHS has now made secondary care medicines data (SCMD) available. You can read the full technical specification of the data here but briefly: it is hospital pharmacy stock control data, which is collected and processed by Rx-Info, and is now published on the NHS Business Services Authority website in the NHS dm+d standard we know, love, and have documented well.

This is the website code for openprescribing.net - a Django application that provides a REST API and dashboards for the English Prescribing Dataset published by the NHS Business Services Authority. Information about data sources used on OpenPrescribing can be found here.

It has been a busy month for paper publication at The Bennett Institute. We have written a brief description of the most recent papers below. Please sharewith colleagues and get in touch if you have any relevant observations! Remember you can read all our academic papers related to OpenPrescribing on our research page.
Hospital medicines data: We are frequently contacted at OpenPrescribing about when we are going to make a hospital version. Unlike primary care, access to hospital medicines data is restricted. The BMJ have just published our Bennett Institute article about why we think The NHS deserves better use of hospital medicines data.
Update May 2021 Based on feedback received from users, the NHS dictionary of medicines and devices has decided to cease maintenance of the “hospital only” value at AMP level (it remains at AMPP level). As a result this means that we are no longer able to produce our “Hospital Only measure” and we have retired it.
Just prior to the COVID-19 emergency we launched a new measure on OpenPrescribing, primary care prescribing of medicines defined by the NHS dictionary of medicines (dm+d) and devices as “hospital only”. In this blog we set out what exactly this means, describe some of our early investigations and interesting (but nerdy) details, and ask for your help in improving and maintaining this dm+d field.

A guest blog from Dr. Kevin Barrett (Twitter @DrKBarrett).
Last week the British Journal of General Practice published our paper on unsafe prescribing of methotrexate. As part of the publication Dr. Kevin Barrett talked to BJGP (see video below) about how he used OpenPrescribing to identify potentially unsafe prescribing in his practice and has also written a short blog below.
When I first started as a GP trainee in 1999 electronic prescribing was a relatively recent innovation. The practice formulary was built by hand, and prescribing analysis only occurred when paper Prescribing Analysis and CosT (PACT) reports were sent to the practice. These evolved into ePACT reports, but these still required time to decipher. With the advent of Primary Care Trust (PCT) and then Clinical Commissioning Group (CCG) employed pharmacists who had the time to analyse the data and present practice- and prescriber-level data to us at a range of meetings we became used to comparing our prescribing data to our peers. Electronic prescribing aids are a useful measure to help guide our prescribing and keep us up to date with the ever-changing local and national recommendations.

This week the British Journal of General Practice published our latest paper on unsafe prescribing of methotrexate. We found that the prevalence of unsafe methotrexate prescribing (10mg tablets) has reduced but remains common, with substantial variation between practices and CCGs. In the paper we also discuss recommendations for better strategies around implementation.
Anyone can view the live data on unsafe methotrexate prescribing at openprescribing.net/measure/methotrexate, to support audit and review in your local organisation. Read the paper here and you can watch Dr. Kevin Barret (twitter @drkbarret) describe here how his practice used OpenPrescribing to identify a breach of their practice policy on methotreaxte prescribing and fix it!
At OpenPrescribing we know that clinicians can be overwhelmed with guidance and data about many different aspects of care. We therefore have developed an innovative email alert service for every single practice, primary care network and clinical commissioning group in England that delivers bespoke custom emails to your inbox about your own organisations prescribing.
To sign up to your organisation’s alerts all you need to do is:
These email alerts help people keep track of their prescribing trends, alert you to changes in prescribing that may be difficult to spot and importantly tell you if your prescribing has changed in comparison to your peers. You can see an example of an OpenPrescribing practice email alert here and you can read more about the methods in our paper.

OpenSAFELY is a new secure analytics platform for electronic health records in the NHS, created to deliver urgent results during the global COVID-19 emergency. OpenSAFELY is a collaboration between the Bennett Institute, the EHR group at London School of Hygiene and Tropical Medicine and TPP who produce SystmOne. OpenSAFELY is now successfully delivering analyses across more than 24 million patients’ full pseudonymised primary care NHS records. The first analysis from OpenSAFELY is Factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients with more answers to important questions expected shortly.
OpenPrescribing.net has been updated this week with the latest release of prescribing data covering March 2020. In-depth analysis will be needed over the coming months, but this release gives us the first glimpse into the impact that COVID-19 has had on prescribing. At the Bennett Institute we have been quite busy with the new secure analytics platform OpenSAFELY but the following blog is a rapid analysis of the March prescribing data which others may find helpful to focus their own investigations. As always, all our analytical code is openly available on our GitHub for inspection and reuse by anyone.

The following is a rapid analysis of the “top 10” medicines in NHS England primary care in 2019. We prepared this analysis for a user who wanted to use the list in a teaching session with students to prepare them for the medicines they will most commonly see in general practice. We are sure others will find it useful — please get in touch and tell us how you use it via Twitter or feedback@openprescribing.net. As always our analysis with complete analytical code is openly available on our GitHub page. You can also investigate the prescribing of any medicines you like using our tools like our Analyse page, chemical trends and our brand new browser for the NHS Dictionary of Medicines and Devices. Read on below where we describe the “top 10” medicines and class of medicines, in terms of volume and cost.

At the Bennett Institute we like to work in the open and share our insights for the whole community, so we can fix a problem for us, then share the solution, and help fix it for everyone. We think this is efficient for us and the whole system. In this blog our magnificent coder Peter Inglesby sets out some analysis he has done of changes to the NHS prescribing data we use. It took us a few hours to investigate these problems for our own purposes, then document our findings and solutions internally; it took an extra 20 minutes to share in this blog post and now we give it to you so you don’t have to replicate our effort and can maybe find some insights we have missed!

Update September 2020: NHS England have announced a reduction in the number of planned measures including the majority of the measures on OpenPrescribing. We will remove the IIF dashboard in a future update.
Update: Due to COVID19 response NHS England has announced that the IIF will be postponed. We will continue to make this dashboard available as NHS England also states that they will continue to monitor the data to understand any impact.

At the Bennett Institute we get many people contacting us every month asking us when OpenPrescribing will be available in their country. In this blog we are outlining OpenPrescribing.yourcountry where we give you the information that you can use locally to build a case for OpenPrescribing in your country and obtain funding to support development. We aren’t quite ready to build OpenPrescribing.yourcountry yet, but we will be soon and we wanted to share our plans so you can be ready when we are.

Most people share their end of year roundup during late December when everyone is too full of cake to read. Now you’re back in the saddle, here’s our roundup of everything the Bennett Institute threw out into the world over the previous 12 months!
OpenPrescribing.net went from strength to strength, with over 135,000 unique users last year. We now have over 80 measures of prescribing safety, efficacy and cost-effectiveness and have been working on new types of measures and alerts to identify “outlier” prescribing, such as with zuclopenthixol. In 2019 we also: launched new dashboards and bespoke alerts for every single primary care network (PCN), sustainability and transformation partnership (STP), and NHS region; upgraded the Analyse page to support more organisations with bespoke medicines queries; and developed tools to help solve the problem of Ghost Branded Generics which cost the NHS an extra £11.6million per annum but has massively reduced during 2019.

Today on OpenPrescribing.net we have launched our Greener NHS prescribing dashboards. Over recent months there has been increasing attention on the environment and the effects society is having on climate change. The NHS announced specific targets as part of its long term plan to become more sustainable, reduce waste and shift to lower carbon inhalers. At OpenPrescribing we have already launched our first prescribing measure related to the environment and this week we are launching our Greener NHS prescribing dashboard for every single general practice, primary care network (PCN), clinical commissioning group (CCG), sustainability and transformation partnership (STP), NHS region and for the whole of England.To access your Greener NHS prescribing dashboard, simply go to your organisation’s measures page and select “Greener NHS” from the drop-down. You can read more about our categories on our blog or watch our short Youtube video.

Today on OpenPrescribing.net we have launched our National Institute for Health and Care Excellence — NICE Prescribing Dashboard. We have a NICE prescribing dashboard for every single general practice, primary care network (PCN), clinical commissioning group (CCG), sustainability and transformation partnership (STP), NHS region and for the whole of England. This allows anyone to explore how NICE guidance has been implemented in their organisation, supporting effective, safer and more efficient prescribing. To access yours, simply go to your organisation’s measures page and select “NICE” from the drop-down. You can read more about our categories here or watch our short Youtube video:

We have now launched our long-awaited Primary Care Networks (PCNs) dashboard, made possible thanks to the the membership list being published by NHS England last week.
We have PCN prescribing dashboards for every single NHS PCN and their member general practices. (Don’t know your PCN’s name? You can find it on your practice dashboard). This allows anyone to explore NHS prescribing patterns in their PCN and how this compares to others across England — supporting safer, more efficient prescribing.

A guest blog from Calum Polwart (Twitter @ShinyBlackShoe)
At the Bennett Institute we value openness and transparency as we believe open discussion of ideas and methods are the key ingredients for high quality data analysis. We think it is unhelpful that so much NHS data analysis is outsourced, or done behind closed doors, as this prevents coalface clinicians from engaging with data and sharing their expertise and insights. We build OpenPrescribing.net, not just for ourselves, but for anyone to explore NHS prescribing data. This democratisation of prescribing data removes gatekeepers and barriers to accessing the data, allows anyone to scrutinise prescribing and produces new insights.

Today on OpenPrescribing.net we have launched our Primary Care Networks (PCNs) dashboard. We have PCN prescribing dashboards available for every single NHS PCN and their member general practices. This allows anyone to explore NHS prescribing patterns in their PCN and see how this compares to other PCNs across England — supporting safer, more efficient prescribing.

Figure 1: South Islington PCN OpenPrescribing Dashboard
PCNs are groups of practices, which together serve communities of around 30,000-50,000 people, with the aim of improving care for patients. PCNs were announced as part of the NHS long term plan and many PCNs have formed already and started to recruit staff such as clinical directors and clinical pharmacists to improve and optimise the use of medicines. We hope our PCN prescribing dashboards will assist everyone across the country to identify and prioritise areas where prescribing can be improved.


Our newest paper is now out in the BMJ! Here we show huge variation in adoption of warranted changes in prescribing behaviour, using some exciting new openly available change detection methods.
This month we have launched a range of new measures. As always, measures are prioritised on your dashboard by potential for improvement so you can quickly and easily spot where your organisation is an outlier. You can also sort by potential savings or group measures by clinical condition.

At the Bennett Institute we regularly collaborate on projects, both small and large, with users who get in touch. For development of this measure we would like to thank the NHS England Sustainable Unit and Centre for Sustainable Healthcare for their input on our work to support the NHS Long Term Plan. Another one of our collaborators on this work is Nicola Read, a respiratory doctor who is currently one of the National Medical Director’s Clinical Fellows. Below we set our new measure on inhalers and the environment and Nicola explains its importance for all inhaler prescribers.

This week we launched a new measure of seven day prescription for medicines used to treat long-term conditions. There is no current consensus on duration of prescription across the NHS and prescribers are advised that they should write a prescription for a duration that is clinically appropriate. For medicines that are for stable long-term conditions many areas have policies in place recommending one, two, or three month prescriptions.
Medicines Compliance Aids (MCAs), sometimes known as dosette boxes or pill organisers, are plastic boxes with small compartments that show which pills need to be taken at what time of day. The British Medical Association reports growing requests to prescribe seven day quantities of medicines to fund supply of medicine compliance aids (MCAs). We propose this measure of seven day prescriptions for long-term conditions as a surrogate measure for MCAs.

Zuclopenthixol is an antipsychotic used for schizophrenia and other psychoses. In the UK, there are two injectable forms of zuclopenthixol:
This week we launched a new measure to support a new type of alert to identify any prescriptions of zuclopenthixol acetate for further investigation. It is not recommended to be prescribed in primary care, so prescriptions may have been prescribed in error.

Following many requests from users, we have created links from our measures to the corresponding search on the Analyse page. This is particularly useful if you want to see multiple practices or CCGs on one chart, view the results on a map, or see exactly which products are included in the measure.
You will notice this is not yet available for all of our measures (which now number close to 100), due to the complex way some measures are constructed. This currently affects just 12 of our standard measures and 4 of the Low-Priority prescribing measures, and we hope to keep increasing the options in the coming months.

This week we have launched a new browser for the NHS Dictionary of Medicines and Devices, better known as dm+d. dm+d is the standard dictionary for the medicines and devices used across the NHS. At last count there were over 150,000 packs of medicines and devices described. You can read more about the dm+d in [this detailed blog]/blog/2019/08/what-is-the-dm-d-the-nhs-dictionary-of-medicines-and-devices/).
We have been using the dm+d browser internally for a while, and having found it very useful we believe it will come in handy for others too, so we have now made it available publicly for anyone to use. Read more about the tool here.

This week we have launched a new browser for the NHS Dictionary of Medicines and Devices, better known as dm+d. dm+d is the standard dictionary for the medicines and devices used across the NHS. It contains codes and descriptions for all these medicines and devices; at last count there were over 150,000 packs of medicines and devices described. You can read more about the dm+d in this detailed blog.
Our dm+d browser allows anyone to search and identify any product in the NHS. For example, you can see all the paracetamol products available in the dm+d here. We’ve previously written about how the dm+d can be useful, like using user-friendly names on the website, or identifying all dry powdered inhalers for analysis. As we have found our dm+d browser so useful, we believe others will find it useful too, and have now made it available publicly for anyone to use.

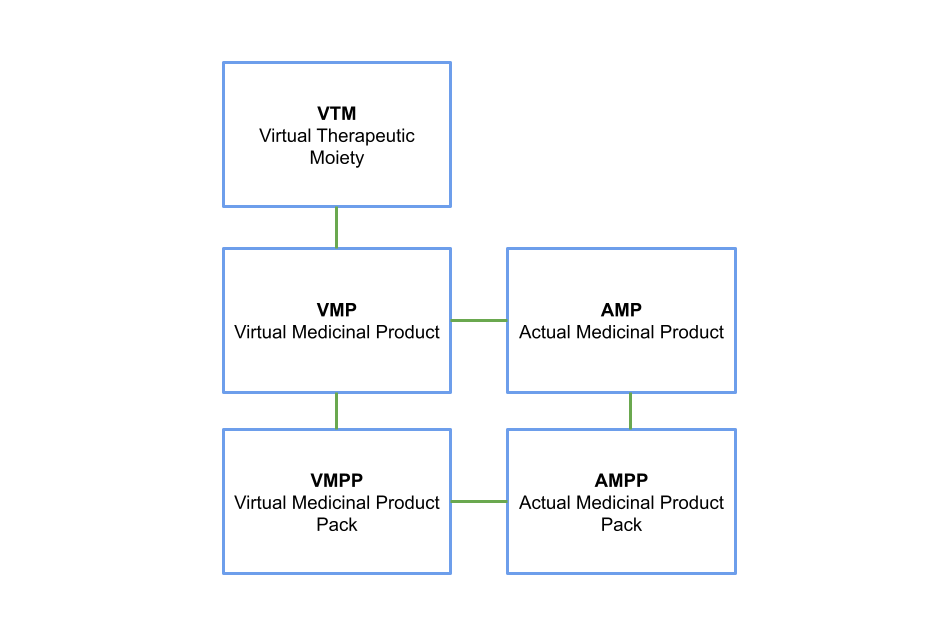
Over the past year we have been increasingly using NHS Dictionary of Medicines and Devices (dm+d). This blog post sets out to describe dm+d for the benefit of the wider prescribing analytics community and others.
dm+d is the standard dictionary for the medicines and devices used across the NHS. It contains standardised codes, descriptions, and metadata (such as price and pack size) for every entry. At last count it contained over 150,000 packs of medicines and devices.

Yesterday (27 June), NHS England completed its consultation on an additional proposed set of products being considered for a recommendation against regular use in primary care. Therefore, on the site we have now included these new items in the set of low-priority measures. The newly added products include bath and shower emollients, higher cost insulin pen needles and dronedarone. See how your practice or CCG is performing on these measures here, or navigate to the Low Priority measures from your favourite organisation’s dashboard.

Our technical team are busy improving how the engine room of OpenPrescribing. When they’ve finished we’ll get them to write a blog on exactly what they’ve done. In the meantime, as the work progresses we are able to add some additional exciting new features to the site.
One of the limitations of how our Analyse page worked was the ability to only search at one BNF level at a time. For example, you couldn’t search for products and presentations together. However, now you are able to add any combinations you want, making this tool much more powerful. For example, it’s helpful when looking at broad-spectrum antibiotics: previously you could only include either cephalosporins and quinolones (BNF paragraphs), OR co-amoxiclav (a BNF chemical). Now you can include all of them at the same time.

Update November 2019: Our NHS PCN dashboards are now live at https://openprescribing.net/pcn/ and you can read more on our launch blog.
Update August 2019: Our amazing developers have written all the code necessary to display all prescribing measures and data for all PCNs in England on OpenPrescribing. Unfortunately there is no national list of PCNs and their membership available, as soon as this is published we will bring you our prescribing dashboards.


One of our recent papers, published in the Journal of Antimicrobial Chemotherapy, highlighted variability in the speed at which different CCGs switched from prescribing trimethoprim to nitrofurantoin (as recommended by PHE for uncomplicated UTI).
It appears that the practices which changed the most were in CCGs that had taken some action to promote the new guidelines, such as a change in formulary. What are the implications? Read more on this in our blog and you can of course see any region’s performance on this measure on OpenPrescribing.

Just before Christmas we had a paper published in the Journal of Antimicrobial Chemotherapy. It looked at how GP practices responded to changes to the guidance for antibiotics for urinary tract infections (UTIs).
It’s an interesting story in itself, but we think that it prompts some wider questions about how GPs are helped to keep up-to-date on guidance on prescribing.
For many years the mainstay of antibiotic treatment of uncomplicated UTIs in women has been trimethoprim. Recently there has been growing concern about the increasing levels of resistance (about a third of urine samples).

This week we have launched a new email alerting service that covers all of NHS England. Many users of OpenPrescribing already receive our monthly newsletter and our innovative email alert service for practice and CCG prescribing measures and for price concessions. We have now developed this service covering all of England based on user feedback. To sign up, just go to the All England page and enter your email address in the box beside the measures categories (see screenshot below).

On OpenPrescribing.net we provide data for individual practices and CCGs (and now STPs and regions!) making it easier for everyone to explore NHS prescribing patterns in England - supporting safer, more efficient prescribing. However, providing data for an individual location in isolation is rarely useful. We need to provide context, so that some sort of judgement can be made about whether the prescribing in question is especially high or low, and how extreme it is, in comparison with others. On OpenPrescribing we do this using deciles. We think providing transparency in our methods is really important, so in this blog I set out our rationale for doing so.

At the Bennett Institute we value openness and transparency as we believe open discussion of ideas and methods are the key ingredients for high quality data analysis. We think it is unhelpful that so much NHS data analysis is outsourced, or done behind closed doors. This blog sets out the steps we take with OpenPrescribing.net to ensure all our analysis and methodology is freely available for inspection, review, and importantly re-use, by anyone. We hope other teams will adopt these approaches so we can all collaborate to optimise analysis, generate insights and improve care for patients in the NHS.

In the last year we estimate that price concessions have cost an additional £165 million in unplanned expenditure for Clinical Commissioning Groups (CCGs), and our OpenPrescribing.net price concession calculator was featured in a major BBC news story and in the Pharmaceutical Journal this week. However, interestingly, NHS price concessions do not just affect the NHS: they also represent unplanned expenditure for charities, local councils, and others. Here, we report our estimate of the impact on non-CCG organisations as an additional £5.6 million in 2018: a huge four-fold cost increase on top of expected prices for a sector that is already over-stretched.

Today we launched NHS regional and STP dashboards on <OpenPrescribing.net>, which allow anyone to see NHS prescribing patterns across areas larger than CCGs. You can find these new dashboards under “Area and Practice Dashboards”.

The NHS across England is now organised into Sustainability and Transformation Partnerships (STPs) and NHS England regions. There are 44 STPs made up of NHS organisations such as CCGs and hospital trusts, and local councils, who developed shared proposals to improve health and social care, whilst ensuring services are joined up across all of the organisations they incorporate. STPs are contained within the five NHS England regional teams; these teams support healthcare commissioning and delivery in their area by providing professional leadership on finance, nursing, medical, specialised commissioning, patients and information, human resources, organisational development, assurance and delivery.

At OpenPrescribing we have a range of prescribing measures that makes it easier for everyone to explore NHS prescribing patterns in England - supporting safer, more efficient prescribing. We now have 70 measures including our two latest on Freestyle Libre and herbal medicines, that we recently blogged about. The measures are available for for every single practice and CCG in England and cover a range of clinical areas such as medication safety and antimicrobial stewardship to support better prescribing.

We have introduced a new email alert service, built upon our recently-launched NHS Price Concession calculator, which shows the cost impact of concessions for every single practice, CCG and for all of England combined.
If you sign up for these new alerts, an email will pop into your inbox soon after a new price concession is announced (approximately once per week) to update you on the impact these costs are predicted to have on your practice/CCG. Read more in our blog, or sign up by going to the price concessions tool from your practice or CCG dashboard.

Ghost Branded Generics are a relatively new category of cost-saving opportunities, caused by prescribers specifying a manufacturer for a generic product, often resulting in a higher reimbursement price compared to the true generic. We estimate the problem costs the NHS £11.6m a year. We have written about this extensively since our first blog on discovering the issue and developed a Ghost Branded Generics dashboard and measure for every practice and CCG in England.

Today we launched a new feature on OpenPrescribing: an NHS Price Concession email alerts service. This is in addition to our existing calculator that shows cost impact of price concessions, which can already be viewed on every practice, CCG and All England dashboard. You can read more about price concessions (aka NCSO) in our previous blogs.
Many users of OpenPrescribing receive our monthly newsletter and our innovative email alert service for practice and CCG prescribing measures. Today we are adding a new NHS Price Concession email alerts service. Once signed up, this alert will pop into your inbox a few hours after a new price concession is announced, which will be approximately once per week, to update you on the impact these costs are predicted to have on your practice/CCG.

…Identify CCG Cost Savings Opportunities using OpenPrescribing.net
Every year in the NHS local teams around the country put together “QIPP Plans”. QIPP stands for Quality, Innovation, Productivity and Prevention and is a large scale programme introduced across the NHS to ensure the NHS delivers more for the same funding. We make no comment on the programme itself but we think OpenPrescribing is a useful tool in helping develop “QIPP Plans” and to identify new areas for savings related to medicines spend.

We have recently released two new measures on OpenPrescribing — the prescribing costs of herbal medicines, and the quantity of Freestyle Libre.
For techie reasons, we’re quite excited about the herbal medicines measure. We don’t like to write measures that require a manually managed list of preparations, as these require a lot of curation, and can quickly become inaccurate if a new drug is released. Therefore for most (if not all) of our measures we use the hierarchical BNF codes provided by the NHS Business Services Authority (you can read more on these here).

While investigating the data behind Ghost Branded Generics, we came across something that we didn’t expect. As part of our work in creating the Drug Tariff viewer (once we’d managed to obtain the data), we’ve got an archive of Drug Tariff (DT) prices going back to 2010. We used our DT archive to compare listed reimbursement prices with what was actually being paid for generics, we sometimes found that the price paid wasn’t the one listed in the tariff. Instead, sometimes the price was based on the drug tariff price…from the future. or to be more precise, one month into the future.

Before Christmas we wrote about Ghost Branded Generics, a very nerdy story about a problem we uncovered that costs the NHS………£11.6million a year. Since then we have launched a freely accessible Ghost Branded Generics dashboard on Openprescribing.net for every practice and CCG in the country; and a Ghost Branded Generics measure so practices and CCGs can track their prescribing of Ghost Branded Generics over time.
We have also had lots of people get in touch about this whole new category of NHS savings. In particular we were contacted by TPP who produce SystmOne, the “electronic health record” (EHR) system used by approximately 40% of GPs in England.

Before Christmas we wrote a nerdy story about Ghost Branded Generics, a problem that costs the NHS £11.6m a year due to prescribers selecting specific manufacturer’s products rather than true generics. This is largely avoidable. Today we launch our Ghost Branded Generics dashboard for every practice and CCG in the country. This can be accessed through every dashboard page (example below) and we think it will be useful to help people change prescriptions from Ghost Branded Generics to true generic prescriptions.

This a very nerdy story about a problem that costs the NHS £11.6m a year. It shows how one small design choice in the software GPs use can have huge ramifications for how we prescribe, and a huge cost impact on the NHS. More than that, it shows how problems like these can only be spotted, and addressed, by mixed teams like ours — doctors, pharmacists, researchers and software engineers — pooling our different skills to build tools and papers.

Each year, we estimate there are up to £5m of Out of Pocket Expenses (OOPE) expenses charged to the NHS, added by dispensing contractors to their invoices. Could some of these expenses be reduced? In 2014/15 NHS Islington CCG wrote to dispensing contractors highlighting such expenses, and from this single intervention achieved a 50% reduction; spread across the country this could amount to a saving of £2.5m.
We’ve done some initial investigations, but don’t have resources to follow up in detail. This post is to note what we’ve found so far. If you are interested in finding out more, and have access to funding, let us know!

In our third full year of existence we produced even more exciting outputs and continued to grow. We welcomed Lydia Berry, back from maternity leave; Dave Evans, Consultant Programmer, who joined the OpenPrescribing technical team; and Brian MacKenna, an Honorary Research Fellow Pharmacist and member of the NHS England Medicines and Diagnostics Policy Unit. We also welcomed Darren Smyth, a UK and European Patent Attorney - our work so far includes our pregabalin papers (here and here), and he has also contributed to our EUCTR work.

At OpenPrescribing we pride ourselves on developing our tools in response to the needs of our users. Last week NHS England announced a new “Do Not Prescribe” list for consultation. Within an hour we made graphs showing every GP practice’s prescribing of these items. You can drill down to CCG level, and then practice level.

We hope that this data will be useful for clinicians and CCG pharmacists to identify where there is most room for improvement, or change. Or, to drive discussion about agreement on the guidance.

This week we launched a new feature on OpenPrescribing, an NHS Price Concession calculator. We show the cost impact of price concessions for the whole of England here and the calculator appears on every single practice and CCG dashboard so you can work out the impact locally.

Price concessions are a short term agreement by the NHS to pay more than the already agreed price for a generic medicine because pharmacists are unable to obtain the generic at its usual price. Regular readers of our blog will remember a series of blogs last year (see archive) where we detailed the issues and this led to the development of our magnificent Drug Tariff and Concession Viewer, which shows the prices over time for each individual drug, automatically updated on a daily basis.

Earlier this week NHS England announced a new “Do Not Prescribe” list for consultation.
Within an hour we made graphs showing every GP practice’s prescribing of these items. You can drill down to CCG level, and then practice level.
We hope that this data will be useful for clinicians and CCG pharmacists to identify where there is most room for improvement, or change. Or, to drive discussion about agreement on the guidance.
The data that drives OpenPrescribing is described briefly in our FAQ. It is supplied by NHSBSA and NHS Digital, and a few other sources.
Over the years we have come to understand the limitations of this data. We’re sharing them here, so researchers can take them into account when carrying out analyses.
When using Practice Level Prescribing Data, bear in mind:
When using list size (e.g. as denominator):

At OpenPrescribing we pride ourselves on developing our tools in response to the needs of our users. OpenPrescribing is being increasingly used at national organisations and we have had many requests for an All England dashboard. This month we launched the first version of the All England dashboard and blogged about it here.

At the Bennett Institute we get many emails about how people are using OpenPrescribing and this month we blogged about how OpenPrescribing can be helpful when medicines are in short supply. Epanutin (phenytoin) 30mg/5ml oral suspension is currently subject to a Supply Disruption Alert and it is very important that patients are identified promptly and their prescriptions are modified if appropriate. To read more about the alert and how OpenPrescribing can be helpful please see the blog here. If you have any other interesting usecases please get in touch at feedback@openprescribing.net

Drug supply issues are an interesting use-case for OpenPrescribing. Here we will talk about a recent example.
Last week the Department of Health and Social Care issued a “Supply Disruption Alert” for Epanutin (phenytoin) 30mg/5ml oral suspension: Pfizer, the manufacturer, will be out of stock of this product from the week commencing 29th October (today) until early December 2018. This means people currently taking Epanutin (phenytoin) 30mg/5ml oral suspension may need to be prescribed a different product.

This week we have launched a new page on OpenPrescribing.net, the All England dashboard, that allows anyone to see the quality of prescribing at a national level. For the first time we have aggregated all the savings from all our measures in one place. For the month of August these numbers are quite staggering:
£13,190,000 - could potentially have been saved if CCGs used our innovative price-per-unit tool (you can read our methods paper here).

Last week, a pharmacist from NHS North Cumbria CCG got our attention by mentioning OpenPrescribing on Twitter. He had just received a letter about a product for treating haemorrhoids called Uniroid. It’s a 50/50 mixture of Cinchocaine and Hydrocortisone, and is also available as Proctosedyl (made by Sanofi), and as a generic (i.e. unbranded) product.
The maker of Uniroid wants North Cumbria to start prescribing Uniroid-branded products, on the grounds it will save the CCG about £11,000 per year.

Recently we created antimicrobial stewardship dashboards for every Clinical Commissioning Group and General Practice in England by grouping our measures (see our blog post here).
We received feedback from users that some of our measures are difficult to understand, because they exhibit a high level of seasonal variation. Antibiotics show the most seasonality amongst our measures (e.g. openprescribing.net/measure/ktt9_antibiotics). As you can see below, it takes a lot of staring at this graph to work out whether the deciles (blue lines) are going up or down overall, and whether the red line (the data from a single CCG) is changing in relation to them.

This newsletter was sent out on Thurs, Jul 26; sign up to receive the next one at www.openprescribing.net
At OpenPrescribing we hide complicated data science “under the bonnet”: we want data to be easy, to come alive and tap you on the shoulder when there’s a problem. As you know we have an “alerts” service, open and free to anyone, that emails you if there’s a new issue with the prescribing at any practice. But how does it all work? Making a tool that sends an alert when a practice hits the highest 10% in the country for a given prescribing measure was easy. But we wanted to spot problems and send alerts much sooner than that: when a practice begins to drift in comparison to its peers over time, well before it becomes an extreme outlier. Our most recent paper shows the inner workings of this service. If you’re really geeky, you can read the paper here. Or you can just sign up and use the service!

Update: You can view a short Youtube video demonstrating this feature here.
On our OpenPrescribing CCG and practice dashboards you can now filter measures by category to view a small group of related measures together.
You can select a category using the new dropdown menu above the measures…

…Or by clicking on a category listed at the bottom of the description of a measure.

Upon selecting a category you’ll see its description / rationale above the measures:

Thanks largely to our new software developer Dave, we are making some improvements to the site.
With the fresh-faced enthusiasm of a new starter, Dave has begun by tackling the various not-so-exciting but still important tasks which we’ve put off doing for ages. These changes are mostly behind the scenes, but you should hopefully notice that the site feels a bit snappier to browse. One of the changes which you can see is that we now clearly label on the site where a practice has closed or become dormant. Due to the way prescribing data is collected, practices can appear to continue prescribing for several months after they become dormant, and so we now flag this up and explain what is happening.

This week our latest paper was published, which describes the trends and variation in prescribing of medicines determined to be of “low-priority” by NHS England. We found that there has been an overall decrease in the prescribing volume of these medications, but despite this, costs have risen slightly. This is driven by higher costs per prescription for drugs such as liothyronine, trimipramine and coproxamol. You can see how much your practice/CCG spends on these items using our measure.

This is a brief blog about something small and trivial, but also big and important.
Recently on the staircase my friend Carl Heneghan came out with a good line about “Patient and Public Involvement”, or “PPI” as it is known in the trade. “People talk about PPI,” he said: “but we need PPPI… patients, the public, and professionals.”
I think this is absolutely correct. In academia, we often fail to focus on what happens at the coalface. In the Bennett Institute we’ve worked hard to change that. We take conventional academic funder money, and health data, and we produce conventional academic papers (by the shovel-load). But we also turn that data and person-time into live, interactive, data-driven tools like OpenPrescribing.net which people can hold in their hands, and use at the coalface to improve patient care.

Our new paper asks the question: Is use of homeopathy associated with poor prescribing in English primary care? The answer, yes. We found that general practices that have worse than average prescribing scores on our standard measures were more than twice as likely to prescribe homeopathy than practices with better than average scores. Interestingly, the level of homeopathy prescribing we found is quite low and is decreasing quite quickly.

The Pharmaceutical Services Negotiating Committee (PSNC) have released 3 sets of price concession price lists for February 2018. Once again, the total amount for England for the month has reduced: we’ve estimated the impact as £9.37 million for February 2018, although this is based on December 2017 data (the latest available at time of writing), and is therefore likely to reduce slightly (as February has fewer days).

The Pharmaceutical Services Negotiating Committee (PSNC) have released 3 sets of price concession price lists for February 2018. Once again, the total amount for England for the month has reduced: we’ve estimated the impact as £9.37 million for February 2018, although this is based on December 2017 data (the latest we have), and is therefore likely to reduce slightly (as February has fewer days).
The total for 2017-18 so far is £308.7 million, although the further impact is probably greater as some formerly low-cost generics are not considerably more expensive. For example levetiracetam 1g tablets, used in epilepsy, were £5.49/60 in July 2017, and in January 2018, following a spell as a price concession, increased to £36.07/tablets.

Here at the Bennett Institute we are a truly multidisciplinary team: clinicians, academics and software engineers, working together to produce tools, as well as papers.
This is glorious fun, and productive. From our time working together as a team we now have software engineers who know about clinical trials, prescribing data, and more; and we have researchers and clinicians who know a bit about building websites.
This may or may not thrill you, but I will share it: our academics write code that runs live on our websites! In addition, our team can be creative, because we all know a little about each others’ work: about what is possible with software and data, and what kinds of problem need solving in medicine.

The latest price concession information for January has been released by the PSNC (in fact, two sets of data in quick succession). The PSNC have also stated that they are “still in discussion with the DHSC regarding further January 2018 price concessions”. Therefore we have made some calculations based on what we know at the moment - as soon as there are changes we will update this blog. For January 2018, on the surface price concessions look better than in previous months, with an estimated impact of about £12.6 million. This brings the total for the financial year to date to approximately £297 million. This is based on an estimated actual cost, using November data for December and January, so there will be slight changes when the actual data is available.

The latest price concession information for January has been released by the PSNC (in fact, two sets of data in quick succession). The PSNC have also stated that they are “still in discussion with the DHSC regarding further January 2018 price concessions”. Therefore we have made some calculations based on what we know at the moment - as soon as there are changes we will update this blog. UPDATE: We’ve now updated the data, both with the final concessions list for January 2018, and the actual cost data for December 2017.

We’ve been thinking in the Bennett Institute about doing stories, using our prescribing data, to go with landmark clinical trials and systematic reviews. Here’s an example.
A new systematic review published this week in JAMA shows that Omega-3 “fish oil” pills don’t really help improve cardiovascular health. As a systematic review, it’s a very useful overview of previous existing research. Perhaps reassuringly, as that evidence accumulated over time, clinicians were already changing their prescribing behaviour. Here’s the long-term NHS prescribing data from our database: NHS doctors gradually began to reduce prescribing of omega-3 a long time ago. Peak omega-3 was 2011!

Everyone at the Bennett Institute wishes you a very Happy New Year!
Unfortunately, the NHS is still having the same problems in sourcing generics. The PSNC announced the latest list of price concessions for December 2017, slightly smaller than November’s, with 86 lines. However, we still estimated a monthly impact for the NHS in December of £27 million, bringing the total excess cost for the nine months to December to £285 million:

Everyone at the Bennett Institute wishes you a very Happy New Year!
Unfortunately, the NHS is still having the same problems in sourcing generics. The PSNC have just announced the latest list of price concessions for December 2017. The list was slightly smaller than November’s, with 86 lines,but we are still estimating an monthly impact for the NHS in December of £27 million. This brings the total excess cost for the nine months to December to £285 million:

Many people I’ve spoken to aren’t aware that gluten-free foods can be prescribed, but it happens quite extensively in an effort to help patients with coeliac disease adhere to a gluten-free diet.
Below is a chart showing the rate of gluten-free product prescribing since 1998, where there is a gradual increase until 2011, when guidance changed to recommend only prescribing of staple foods such as bread and flour. Recently there has been a sharper decline.

In our second full year of existence we produced even more exciting outputs and continued to grow. You can see the team on our website: Emma-Jane has been our project manager since the Spring; we have two new part-time coders working for us; and researchers Alex, Nick, Daniel and Karolina all started this year. We’ve delivered a range of great new features on OpenPrescribing, got great progress on numerous pre-launch projects, and have a nice portfolio of papers submitted.

We’ve taken a quick look at the data to see why, despite the number of price concession lines have increased to 91 in November, the estimated total excess cost has reduced. (Reminder - we’ve used September prescribing data to estimate the effects, as that’s the latest data available).
The full table is below, but here are some highlights:
As always, you can find our Drug Tariff viewer at www.openprescribing.net/tariff. We’d love to know what you think about the work we’re doing, or anything to do with the OpenPrescribing tool. Please let us know on Twitter, our Facebook page, or via email at feedback@openprescribing.net.

The PSNC has published the list today of Price Concessions for November 2017. The list is the biggest yet, at 91 lines.
We’ve taken a first stab at calculating the estimated effect for CCGs, using September 2017 prescribing data. The Google Sheet can be found here. (edit) - the Google Sheet now also contains national calculations per presentation and all CCG presentation data.
A couple of calculation changes:
The total for England (actual cost) for November is £38.5m. We’ll do some further calculations when we get the chance. It’s less of an impact than we were expecting - possibly as some of the “big excess” items have been removed. We’ll take another look tomorrow!(edit) - we’ve taken a quick look - and here are some of the reasons why the total cost of price concessions is lower.

We have been writing a lot recently about the effect of price concessions on the NHS primary care drugs bill, and on the problems community pharmacy are facing.
We’ve been asked for some CCG-level data, and so here it is; both for the confirmed data for April-September 2017, and for an estimate for October, which is based on October price concession data with September’s prescribing data.
(edit) We’ve also been asked how the costs were calculated. We calculate the difference in the unit cost, i.e. (price concession cost per pack - DT cost per pack)/pack size and then multiply by the prescription quantity for each affected presentation. Please note that these calculations are based on Net Ingredient Cost (NIC) not Actual Cost, and so the impact to CCGs will be slightly lower (about 7%).

Today we’ve released our new Drug Tariff viewer. It was a dataset that we previously didn’t hold, but thought that it would be useful to turn into a graphical viewer for people to use to see how the reimbursement price on drugs changes over time, and also to use as the basis of the effect that price concessions are having on the NHS.
However, obtaining and normalising the data proved to be a bit of a challenge.

The Drug Tariff, published on behalf of the Department of Health and updated monthly, is a strange and mysterious document, written largely in legalese, and understood by pharmacists and almost no-one else. Ask a GP where they find out the cost of the drug, and they’ll say either their computer system or the BNF. For pharmacists, it’s usually the Drug Tariff (or the Tariff). And that’s usually where the most accurate price will be found.

There has been an interesting and concerning story in The Times today regarding shortages on a number of commonly-used medicines and a corresponding increase in the costs.
Here at OpenPrescribing we have been taking a look at these data as well, and trying to estimate to the cost to the NHS this year.
As the Times article suggested, the excess costs are now hitting £50m per month, with £175m extra spent in primary care by September:

One of the most common requests we receive is to be able to use the analyse page without needing to select a denominator, so that you can simply see how much of a drug is being prescribed in each CCG or practice. We’ve now made this feature available. When creating an analysis, simply select “nothing” in the versus dropdown, and you can then see raw monthly data for each practice or CCG.

We have created a new interactive tool for exploring the national Prescribing Cost Analysis (PCA) data, allowing you to investigate prescribing trends over 19 years from 1998 to 2016.
We’ve done a huge amount of hard work to make this tool simple and easy. For example, lots of drug names have changed over time, treatments have moved between Chapters of the BNF, or been assigned new codes. We have “normalised” the data (by hand!) to take account of all this, so we can show each drug according to its current position in the latest BNF dictionary. We have also taken account of changes in national population, and even corrected all prescribing costs to 2016 pounds sterling!

We have created a new interactive tool for exploring the national Prescribing Cost Analysis (PCA) data, allowing you to investigate prescribing trends going back to 1998. The PCA data contains annual data on all drugs dispensed in the community in England. Note this makes it slightly different to the monthly dataset used elsewhere on OpenPrescribing which shows how items were prescribed in England. This means that, for example, in PCA data generic products will not appear until the generic is available to be dispensed, and prescriptions written in Wales will be included provided they were dispensed in England.

We send out monthly newsletters for OpenPrescribing, detailing new features and updates, which you can sign up for here. Our latest issue is below:

NHS England recently launched a consultation on new prescribing guidelines, which lists treatments that should generally no longer be prescribed. We have launched a new tool that allows you to explore the prescribing of these ’low value’ items in any GP Practice or CCG in England.

Today we launch another exciting new feature on OpenPrescribing. NHS England recently shared a list of 19 classes of treatment which they think should not be prescribed by GPs. These treatments were advised against on the grounds that they are ineffective, and therefore wasteful, or at least “low priority”.
We think it’s good for everyone to be able to see what GP practices are prescribing: the GPs themselves, but also patients, journalists, commissioners of health services, the public, medicines optimisation teams, and indeed anyone who is interested in exploring and improving healthcare.

Today we launch another new feature on OpenPrescribing. As you will probably know, we have various standard prescribing measures which show how a practice or CCG is prescribing in comparison with their peers. These are presented as percentages or rates, and often the maths is very simple: what is the proportion of “undesirable drug” divided by “all drugs in that class”. But sometimes there are lots of drugs in the “numerator”, the top half of the equation. For these measures, if a practice is doing badly, we wanted it to be easy for everyone to see exactly which drugs are contributing to that score.

At OpenPrescribing, we provide tools for analysing prescribing behaviour in primary care in the NHS in England. If you work with prescribing data, you may have noticed that practices which are “dormant” apparently continue to prescribe. This short article explains why, for the curious.
Our prescribing data comes from the NHS Business Services Authority (NHSBSA), who are responsible for processing dispensing information supplied by pharmacies. Each line of the data includes a practice code which uniquely identifies the GP Practice that issued the prescription. To understand more about each practice (including its contact details, location, and CCG membership), we cross-reference this code with GP Practice data published by NHS Digital. That data contains a column, status, which sometimes contains the value D, for dormant.

Today we are launching something very exciting: a new tool that identifies over £100m in new prescribing cost savings for the NHS. The average practice can save £50,166 a year by using our tool. These are vastly bigger savings than any other current advice such as “always prescribe generically”. You can use the tool right now, online, for free, at our OpenPrescribing.net service: just look for the “experimental measures” link on any CCG or GP practice page. You can also read our preprint paper describing the extent of the NHS savings, and more detail on the technical background, here; and also our detailed FAQ on various technical matters here.
Recently, we’ve been experimenting with integrating the Dictionary of medicines and devices (dm+d) into our prescribing data. dm+d is the standard dictionary for the medicines and devices used across the NHS, and it contains codes and descriptions for these medicines.
There are several benefits to using dm+d; the most useful side-effect is to allow us to show user-friendly names for drugs. The canonical names for drugs in the NHS prescribing data are sometimes very hard to read. They are taken from the NHS’ own version of the British National Formulary, which uses heavily truncated names, full of abbreviations, so they can fit within an arbitrary 15-character limit.

We’ve recently added the option to download your results from the Analyse searches you complete on OpenPrescribing.
There are now three ways to download data from the site. We do also offer free custom extracts, so if there is anything you are struggling to get from the website yourself send us an e-mail.Update: Due to resource limitations we are no longer able to offer free custom extracts.
If you download and use any data from OpenPrescribing please link back to us or cite us.

OpenPrescribing takes open datasets from NHS Digital and NHS Business Services Authority, and makes it easy for people to explore the prescribing dataset. We also use this dataset in our research, and offer bespoke data extracts from the prescribing dataset for researchers, clinicians and NHS staff (get in touch!). In this series of blog posts we’ll explain key concepts and share our knowledge of the prescribing dataset. In the first blog, we take a look at BNF codes.

Today NHS England announced it is reviewing the prescribing of medicines which it deems to be “ineffective, unnecessary [and] inappropriate for prescription on the NHS”.
We make no comment here on whether it is a good or a bad idea for the NHS to stop prescribing these items. We are keen that everyone in the NHS should use data better, to help understand who is prescribing what, and below we show how you can use OpenPrescribing to investigate the prescribing of these items in your area.

We launched our e-mail alerts on OpenPrescribing to help people keep track of prescribing trends at their GP Practice or CCG. Our alerts send you a monthly e-mail highlighting any new signals in our prescribing measures (including the new measures we launched this month!). This will help you keep track of changes in prescribing, as our alerts can help you find changes that might otherwise be difficult to spot by eye.
You can sign up to receive alerts for any GP Practice or CCG in England by going to the dashboards and entering your e-mail address. We will then send you monthly updates tailored for the practice or CCG you are interested in.

We’ve been spending some time at OpenPrescribing designing a set of new measures to identify interesting variations in prescribing behaviour across the country.
We’ve talked to people from CCGs, and have looked (via Freedom of Information requests) at a number of CCG schemes for improving prescribing, and have come up with a number of areas that we think are important.
Some, like the opioids measure, are important for both cost and clinical reasons. Others, such as the glaucoma measure, show where there is prescribing by brand, which we don’t think is necessary. We also have measures, like generic diltiazem, which show where we think there is prescribing which doesn’t meet national guidance on how they should be prescribed.

OpenPrescribing was featured in a recent TARGET antibiotic webinar, which shows how you can use the site to explore antibiotic prescribing in your local CCG or GP practice. It looks at the antibiotic measures featured on our CCG & GP practice dashboards, and how to construct your own queries on the Analyse page.
The webinar demonstrates a range of tools that can be used to take an in depth look at antibiotics - and OpenPrescribing is featured from 5:30. If you want to have a go at using the Analyse page yourself (to look for antibiotics or any other drug!) we’ve written some guidance here.

In our first full year of existence we’ve grown fast, recruiting lots of new staff. You can see us all on our new website: Lydia our project manager started in the Spring, as did Seb, our new coder; Lisa, our community engagement manager, started over the summer; Helen, our new researcher, started in December, with two more researchers starting in January. For our OpenPrescribing work we’ve been joined by Richard as our pharmaceutical advisor. We’ve also been lucky enough to pull in a huge team of excellent students including Jess, Sarah, Mark, and the mighty COMPare project team of Henry, Aaron, Ioan, Philip, and Eirion. We’ve now delivered some of our early projects, and have a nice portfolio of papers submitted already.

How do you know if your product is really working for users? You can guess, you can ask them, or best of all, you can watch them actually using it.
With OpenPrescribing, we want to make it easier for Clinical Commissioning Groups (CCGs) to monitor prescribing behaviour, and for GPs to prescribe in the best way. So it’s important that it really does help those users do those things. And the only way to verify that is with user research.