Investigating weight gain and obesity with OpenSAFELY
- Posted:
- Written by:
-
- Miriam Samuel
- Categories:
This article is part of a series: Guest Blogs
- High Dose Dexamethasone
- How I use OpenPrescribing in my practice as a GP
- Conducting Research Using OpenSAFELY: My Experience of the Co-pilot Service
- Using electronic health records and open science in the COVID-19 pandemic
- Exploring the Impact of COVID-19 on common infections: Treatment Pathways, Antibiotic Prescribing, and Exposure
- Incidence and management of inflammatory arthritis in England before and during the COVID-19 pandemic
- Updates of OpenSAFELY Research on COVID-19 Therapeutics
- Understanding Repeat Antibiotic Prescribing in the Pandemic: Insights On Health Inequalities
- Trends in inequalities in avoidable hospitalisations across the COVID-19 pandemic
- Prescribing of Lidocaine Plasters
- The safety of antivirals and neutralising monoclonal antibodies used in prehospital treatment of Covid-19
- Investigating weight gain and obesity with OpenSAFELY
- Optimising Antibiotic Use in Primary Care
This is a guest blog by Miriam Samuel from Wolfson Institute of Population Health at Queen Mary University of London.
We used OpenSAFELY to investigate how the COVID-19 pandemic impacted the weight of adults living in England, and found significant inequalities in the patterns of weight gain in different groups of people. Women, younger adults, people living in deprived areas, and people with a history of mental health conditions were at greatest risk of rapid weight gain, while the pandemic was at its peak.
We can all remember what it was like during the lockdowns. They were essential, of course, to control the spread of the virus. But even so, there’s growing evidence that pandemic restrictions like lockdowns had a negative impact on other aspects of physical and mental health.
Our team - from Queen Mary University of London, University College London, Imperial College London, the University of Leicester and the Bennett Institute - have been working together since early 2022, to understand what happened to the weight of adults living in England during the pandemic.
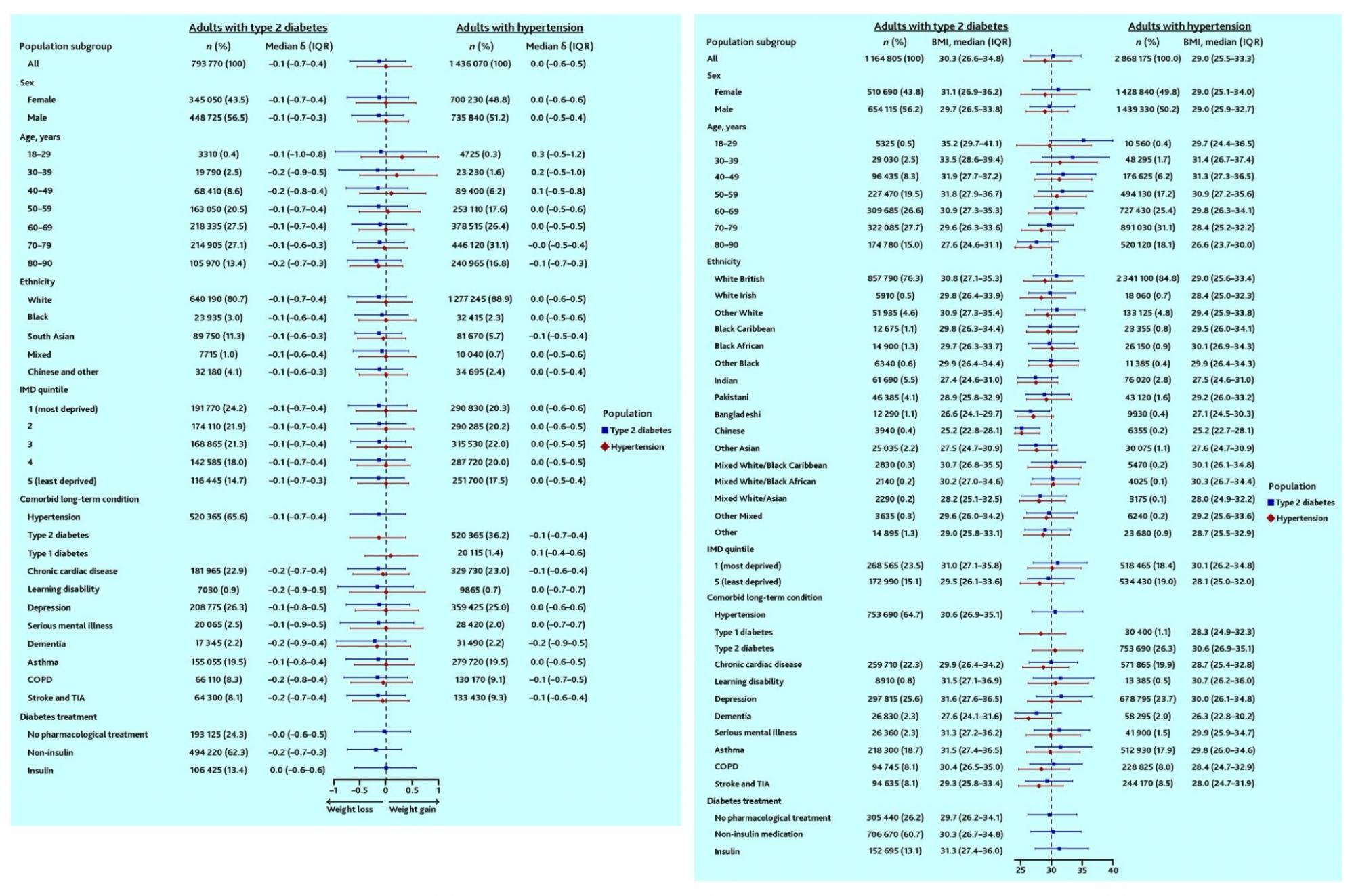
We recently published the second of two papers. Using OpenSAFELY, we looked at data from adults in England: 3.6 million with hypertension (high blood pressure) and 1.2 million with type 2 diabetes. We picked these conditions because they’re closely related to body weight. We wanted to see which groups of people living with these conditions were most at risk of unhealthy weight gain during the pandemic.
We found that, amongst adults living in England with type 2 diabetes, just over half (56%) were obese, compared to just under half (45%) of those with hypertension. On average, adults with type 2 diabetes lost weight during the pandemic. Those with hypertension managed to maintain a stable weight.
But these overall trends disguised significant inequalities in patterns of weight gain on an individual level: about 21% of people with diabetes, and 25% of those with hypertension gained weight rapidly. Women, younger adults, those living in more deprived areas, and individuals with a history of mental health conditions were at greatest risk.
In another paper published earlier in 2024, we’d investigated weight trends amongst all adults registered with a GP in England, not just those with type 2 diabetes or hypertension. Once again, women, younger adults, those living in more deprived areas and those with a history of mental health conditions were most likely to gain weight rapidly, and experience extreme acceleration in their rate of weight gain during the pandemic.
Using routine data for far-reaching insight
The point here is that the pandemic, and the essential restrictions that came with it, had a more negative impact on the health of some groups than others.
Health inequalities that existed before the pandemic were likely to be exacerbated during the pandemic. Understanding who was at greatest risk of unhealthy patterns of weight gain during the pandemic can help us target weight management interventions to reduce the long term impact of these health inequalities.
From a medical science perspective, this work has also shown how useful OpenSAFELY can be as a tool for studying routinely-collected data to generate insights that are far from routine. Our team was able to access anonymised historical and near real-time data on the weight of millions of individuals registered with a GP in England. We focused on weight recorded in the GP health records between March 2015 and March 2022, but more data were available! By using anonymised data from GP health records we were also able to gain an understanding of what happened to the weight of adults living with different health conditions. There’s lots more to find out, and our work on this project will make a small contribution to projects that follow on from it.


